Special Offers
At Southard Family Dentistry, we are committed to helping each patient receive the treatment they deserve.
Offers Expire: April 30th, 2024
Your Best, Healthiest Smile
At our practice, each patient is treated with highly individualized dental care designed to best meet their needs. Your health and comfort are our top priorities, and our goal is to help you feel and look your very best.

TMJ Specialist
Southard Family Dentistry is a practice that focuses on state-of-the-art treatment for TMJ. Dr. Heather Bond-Southardhas completed extensive training in the treatment of TMD disorders, and is eager to use her expertise to help all those who suffer from TMJ/TMD.

In-House Dental Savings Plan
We're proud to help our patients afford the dental care they need each year with our in-house dental savings plan! Your annual membership includes two free dental cleanings with x-rays, along with deep savings on the dental restorations you need, for just $189. Save even more when you add a family member to your plan!
Featured Services
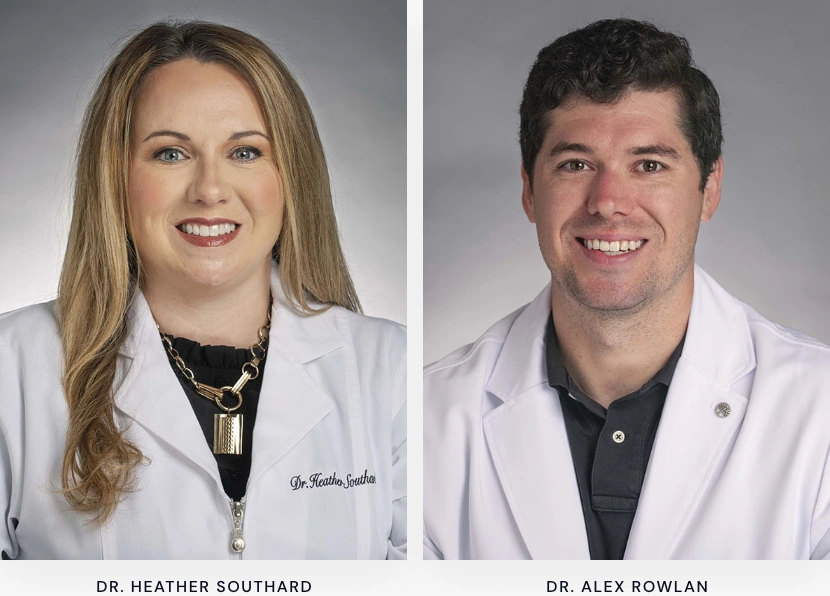
Meet Your New Dentists
Our dentists offer expertise in a wide variety of services that are delivered with each patient's best, healthiest smiles in mind! With our friendly, knowledgeable team, patients can achieve a long list of oral health and aesthetic goals in one place.
Visit Us Today
2600 Browns Ln, Jonesboro, AR 72401- Monday:
- 8:00am - 5:00pm
- Tuesday:
- 8:00am - 5:00pm
- Wednesday:
- 8:00am - 5:00pm
- Thursday:
- 8:00am - 5:00pm
- Friday:
- 8:00am - 3:00pm*
*We are open every other Friday. Call our office for details.
Visit Us Today
2600 Browns Ln, Jonesboro, AR 72401- Monday:
- 8:00am - 5:00pm
- Tuesday:
- 8:00am - 5:00pm
- Wednesday:
- 8:00am - 5:00pm
- Thursday:
- 8:00am - 5:00pm
- Friday:
- 8:00am - 3:00pm*
*We are open every other Friday. Call our office for details.